In general, inflammation refers to the body’s natural response to an offending agent, such as tissue damage or injury, or infection, which involves the recruitment of mononuclear leukocytes (monocyte and lymphocytes). Acute inflammation relatively occurs in short duration, lasting for a few hours or days, depending on the severity of the injury and generally a controlled inflammation that benefits the body by protecting against tissue damage or any harmful agent. In contrast to acute inflammation, chronic inflammation lasts for a prolonged period such as a few months, years and even a lifetime.
What happens if inflammation left untreated?
Chronic inflammation, if left untreated, would trigger your body to persistently produce inflammatory chemicals, causing long-term damage to healthy cells. Of grave concern is chronic inflammation has an established association with chronic diseases such as cardiovascular diseases and type 2 diabetes (figure 1).
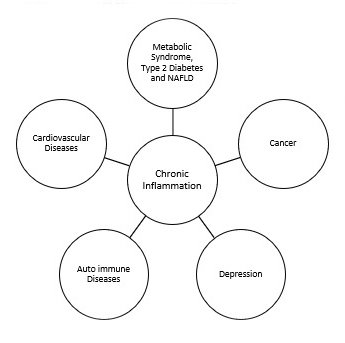
Figure 1: Consequences of chronic inflammation
Chronic diseases kill 41 million people yearly, accounting for 71% of global total mortality, according to the World Health Organization. Chronic diseases, also known as noncommunicable diseases, are distinguished by their long latency period and multifactorial nature, which includes genetic, behavioural, and environmental factors (table 1).
| Genetic | Behavioural | Environmental |
| Gene mutation | Tobacco use, exposure to secondhand smoke | Air pollution, water pollution |
| Unhealthy diet | Ultraviolet radiation | |
| Physical inactivity | Endocrine-disrupting chemicals | |
| Excessive alcohol consumption | Persistent organic pollutant |
Table 1: Factors of chronic diseases
How to measure it?
Chronic inflammation is a silent killer. It has no obvious symptoms or indications until it interferes with and damages healthy cells. Measuring inflammation is not as simple as measuring our weight on the scale. It is multifactorial, necessitating expert interpretation. A single test result should not be used to diagnose the inflammation condition. However, as a “guide”, inflammation can be measured by observing inflammatory markers* such as erythrocyte sedimentation rate (ESR), c-reactive protein (CRP) and plasma viscosity (PV) via a blood test. Always seek the advice of a professional when interpreting the results.
Erythrocyte Sedimentation Rate (ESR) test
ESR test measures how quickly red blood cells fall or settle at the bottom of a test tube containing a blood sample. This process of “falling” or “settling” is called sedimentation. The faster the sedimentation rate, the higher the levels of inflammation in the body.
- Normal range**:
- Men: 0 – 10 mm/hr
- Women: 0 – 20 mm/hr
C-reactive protein (CRP) test
- CRP is a protein synthesized by the liver and is released into the bloodstream in response to inflammation. A high level of CRP in the blood indicates there is inflammation or infection in your body.
- Normal range**:
- 10 mg/L
Plasma Viscosity (PV) test
- Alongside ESR and CRP tests, PV can be used as a marker of inflammation. PV is used to access the viscosity or thickness of blood and indirectly measures the protein content in the plasma (liquid) part of the blood. A higher-than-normal PV value may associate with the inflammation state.
- Normal range**:
- 1.50 – 1.72 mPa.s
*A number of conditions could affect the level of inflammation markers. Thus, its interpretation requires careful assessment by clinical practitioners and physicians.
**These normal ranges may vary slightly difference between laboratories.
Preventing inflammation
While inflammation is necessary for the body’s defences, chronic inflammation may increase the risk of various diseases. The best advice to curb inflammation is to live a healthy lifestyle.
References
Brigden, M. (1999). Clinical utility of the erythrocyte sedimentation rate. American Family Physician, 60, 1443–1450.
Brigham and Women’s Hospital. (n.d.). Environmental Risk Factors for Chronic Disease . Retrieved January 25, 2022, from https://www.brighamandwomens.org/research/departments/channing-division-of-network-medicine/environmental-risk-factors-for-chronic-disease
CDC. (n.d.). About Chronic Diseases . Retrieved January 25, 2022, from https://www.cdc.gov/chronicdisease/about/index.htm
Furman, D., Campisi, J., Verdin, E., Carrera-Bastos, P., Targ, S., Franceschi, C., Ferrucci, L., Gilroy, D. W., Fasano, A., Miller, G. W., Miller, A. H., Mantovani, A., Weyand, C. M., Barzilai, N., Goronzy, J. J., Rando, T. A., Effros, R. B., Lucia, A., Kleinstreuer, N., & Slavich, G. M. (2019). Chronic inflammation in the etiology of disease across the life span. Nature Medicine 2019 25:12, 25(12), 1822–1832. https://doi.org/10.1038/s41591-019-0675-0
Mayo Clinic. (2021, June 25). C-reactive protein test. Circulation; NLM (Medline). https://doi.org/10.1161/CIR.0000000000000678
Wehby, G. L., Domingue, B. W., & Wolinsky, F. D. (2018). Genetic Risks for Chronic Conditions: Implications for Long-term Wellbeing. The Journals of Gerontology: Series A, 73(4), 477–483. https://doi.org/10.1093/GERONA/GLX154
